CategoriesPsoriasis Treatment
CategoriesPsoriasis TreatmentLiving With Psoriasis
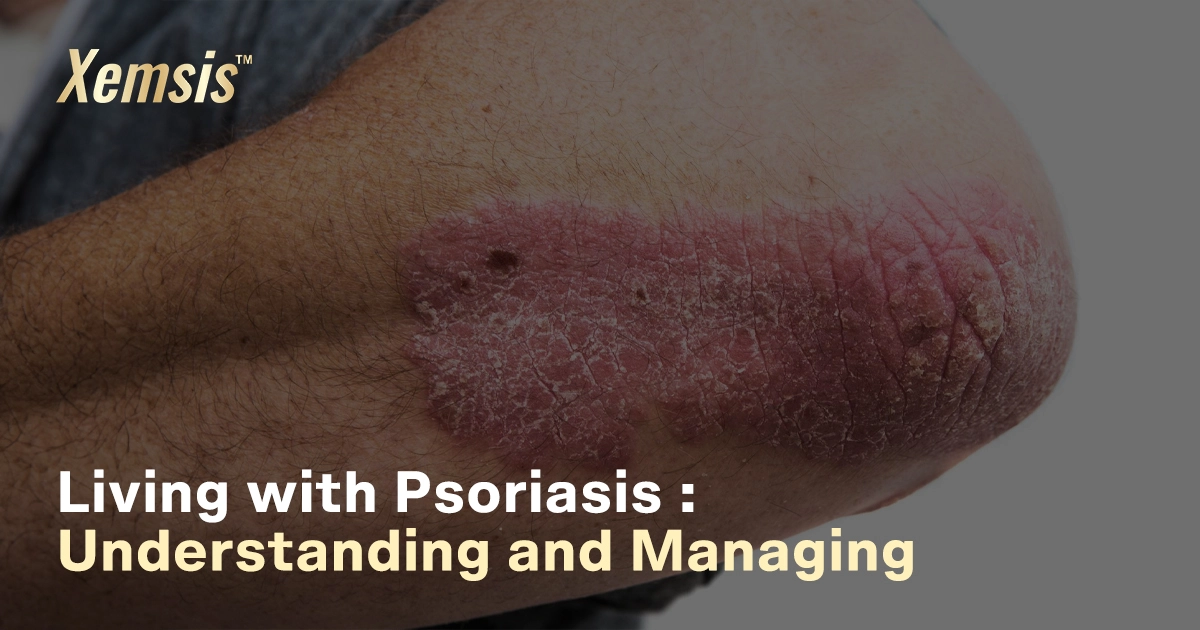
Dear Warriors
Living with psoriasis may not be an easy task. It may last longer and cause severe flare-ups, physical discomfort, and emotional challenges. The symptoms may sometimes be severe and painful. Though you know psoriasis isn’t contagious, you would still prefer not to expose the symptoms, as it looks severe and infectious. But I want to remind you today that you are stronger and prettier than you think. Your worth as a human being isn’t tied to your clear skin or facials.
Accept your Struggles
First and foremost, let’s accept the reality of living with psoriasis. It does affect your quality of life, self-esteem, and even your relationships. It’s okay to be frustrated. But you are not alone in this fight. Yes, you are a part of the 125 million people globally who suffer from psoriasis. You deserve to be happy. Keep calm, stay positive, and maintain your physical health consistently. You can also try speaking with people who had psoriasis and how they overcame the stress and pressure.
Support your Strength
Every challenge you face from living with psoriasis, every flare-up you manage, every treatment you undergo, and every time you step out confidently will showcase your bravery to the world. Concentrate on your work rather than confining yourself in the home with stress and depression. Be an inspiration to other people with psoriasis. The best way to overcome your worst nightmare is to face it. Once you achieve something, the world will not see your condition. But it will be inspired by your strength and how you rose above your struggles.
Be a game-changer
Living with psoriasis can be a part of your life. But it can’t control your narratives. Write your own inspirational story today. Find the beauty of your journey through psoriasis and inspire the community of millions of people who face struggles and challenges regularly in their lives.
Hope and Healing
Never lose your hope. Be in touch with your healthcare provider and follow his guidelines regularly. Maintain a healthy diet, engage in physical activities, avoid alcohol and tobacco products, spend time with your loved ones, and stay hygienic. Following preventive measures and staying positive can surely help you keep psoriasis symptoms at bay.
How can Xemsis help?
Xemsis is formulated after many years of research and is made with 100% pure natural ingredients to treat all forms of psoriasis and seborrheic dermatitis. With safety and quality as a top priority, the ointment has no added steroids, parabens, or toxins to avoid the risk of side effects.
After applying Xemsis, the ointment’s rich ingredients slow down the immune system’s excess production of cells. This decreases the formation of plaques and reduces inflammation on the outer side of the skin. You can see a visible reduction in the symptoms of psoriasis in just 7 days of ointment usage.
With 30 years of excellence in providing effective psoriasis treatment, Xemsis has now spread to various states of India and is recommended by many doctors to treat psoriasis. We have received over 15,000 orders in the last 3 months and have satisfied many customers with our treatment of psoriasis. Check out our website to learn about the feedback of our satisfied customers.
Final Note
To every warrior battling psoriasis: You are more than your skin. Your skin won’t determine your worth, strength, or beauty. With all the ups and downs, keep your motivation high and keep moving forward. Remember that you are not alone in this battle. Bring hope to people with psoriasis through your inspirational journey, story, and strength.
With heartfelt regards and support
Xemsis: Your all-in-one, ultimate solution to psoriasis