Psoriasis in the Ears: Symptoms, Treatment, and Care
Psoriasis in the ears is a rare and auto-immune condition that affects the outer and inner parts of the ears. The condition is chronic, as dead skin cells accumulate largely in the affected areas. The accumulated dead cells affect the skin in the form of scales or wax, which blocks the ear canal, leading to temporary hearing loss, which is medically termed sudden sensorineural hearing loss. Treatments are available to prevent hearing loss and severity.Overview
What is psoriasis in the ears?
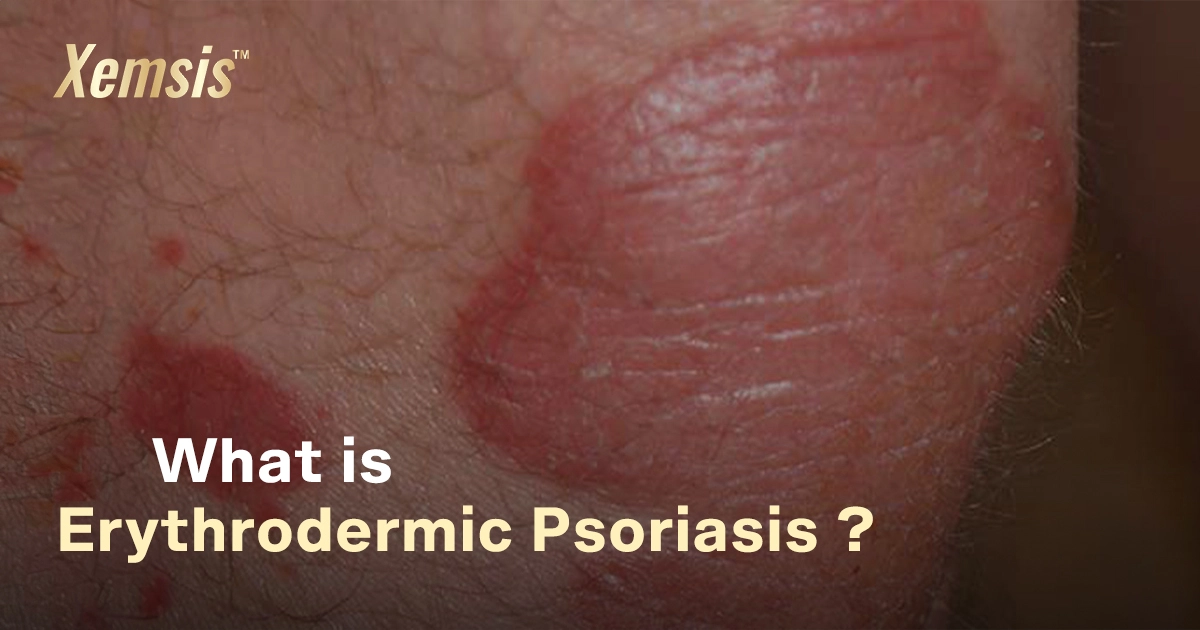
Psoriasis is a chronic skin condition that occurs in different forms in various parts of the body. But psoriasis affecting the ears is a rare condition. It can affect any region of the ears, like the ear folds, ear lobe, inner ear (ear canal), or outer region of the ear. However, psoriasis won’t spread deep inside the ears and won’t affect delicate parts like the eardrums, which can lead to permanent hearing loss. Psoriasis in the ears can range from mild to severe, depending on the condition.What types of psoriasis affect my ears?
Many types of psoriasis can affect the regions of the ears. The forms of psoriasis that affect the ears more commonly are:-
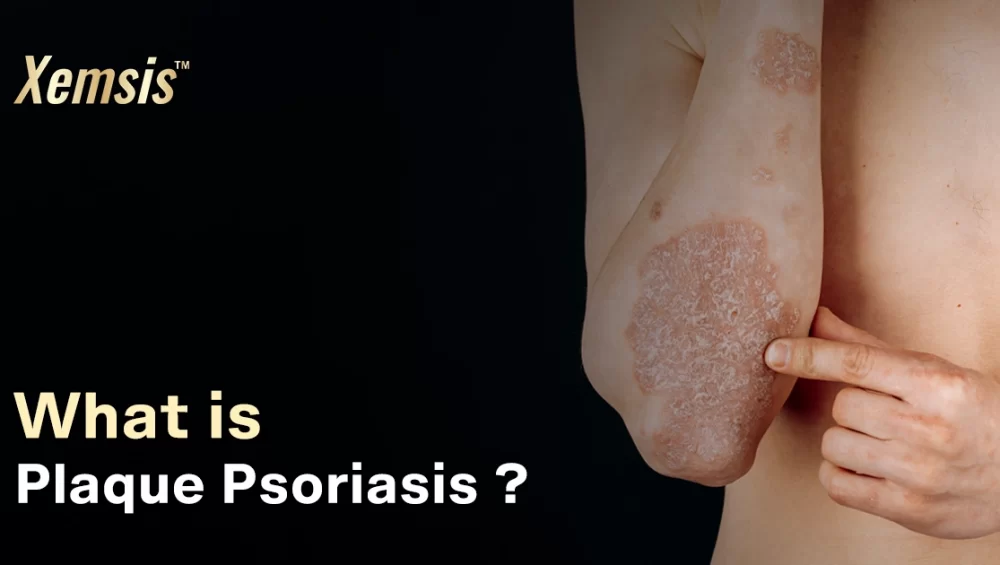
- Plaque Psoriasis: This type of psoriasis affects the inner or outer regions of the ears as thick and scaly patches that are itchy and reddish.
- Inverse psoriasis: This type of psoriasis affects particularly the ear folds as inflamed and itchy plaques.
- Sebopsoriasis: This type is a condition where psoriasis and seborrheic dermatitis occur together. This form causes pus-filled bumps and yellowish-scaly plaques in the inner or outer regions of the ears.
To whom does psoriasis affect the ears?
Ranging from children to adult men and women, anyone can get affected by psoriasis in the ears. However, people who are affected by other forms of psoriasis or have a genetic history of psoriasis have a higher risk of developing the condition.Is psoriasis common in your ears?
Psoriasis in the ears is very rare, as most psoriasis affects parts like the hands, legs, back, scalp, and neck. Though it is rare in the ears, there are higher chances of developing psoriatic flare-ups in other parts of the body if you are already suffering from psoriasis.Difference – psoriasis and eczema in the ears?
Both eczema and psoriasis cause similar symptoms of reddish and itchy plaques in the ears. Eczema is a common condition that can affect any region of the body, including the ears. Psoriasis is a complicated condition that can affect any person on any part of the body. Psoriasis in the ears is mostly experienced by people who are already suffering from other forms of psoriasis, but eczema in and around the ears is mainly caused by genetics, poor environmental factors, or other infections. In terms of symptoms, psoriasis in the ears causes flaky and scaly plaques. On the other hand, eczema in the ears causes small bumps and excess dryness. It is very hard to differentiate between these similar conditions on your own. Only experienced doctors can differentiate it thoroughly.Symptoms and Causes
Symptoms of psoriasis in the ears
Symptoms of psoriasis in the ears mostly look like a patch that is itchy, scaly, discolored, and dry. The symptom causes a burning sensation and is medically called plaques. Scratching these affected areas will worsen the symptoms of bleeding and inflammation, which can also affect the nearby areas. The formed plaques usually accumulate largely in the affected areas and cause blocked ears or temporary hearing loss. Psoriasis in the ears also has a higher chance of spreading to other areas of the face like the eyes, mouth, and nose. In more complicated cases, it may also spread to the lips, tongue, and gums inside the mouth.Causes of psoriasis in the ears?
The exact cause of psoriasis in the ears is not proven yet. However, the chemical process behind the condition is that it causes the immune system to overreact, which leads to the rapid production of new skin cells. For a healthy person, the skin cells usually shed and grow every 30 days. But for people with psoriasis in the ears, these new skin cells grow rapidly in 3 to 4 days. As the process is very quick, the dead skin cells accumulate on the surface of the skin instead of shedding. These accumulations affect the skin, causing inflammatory patches on it. Other conditions that trigger psoriasis in the ears include:- History of family genetics with psoriasis
- Overdosage of certain medications
- Any severe infections from microbes
- Excess stress
- Severe sunburn
- Affected from other forms of psoriasis
- Drinking too much alcohol
- Smoking
- Poor environmental factors
Can psoriasis in the ears cause hearing loss?
Psoriasis in the ears mostly affects the outer parts and ear pathways known as the ear canal. So the dead cells accumulate largely as psoriatic plaques, which block the ear and cause temporary hearing loss. This hearing loss can be treated with treatments. However, if the symptoms of psoriasis become severe and develop into psoriatic arthritis, it can affect the inner regions of the ear and cause permanent hearing loss. So it’s essential to consult with a doctor in the early stages.Diagnosis and Tests
How is psoriasis in the ears diagnosed?
Initially, the doctor would diagnose the condition of your symptoms, followed by examining your complete medical history, including genetics. If there are excess dead skin cells blocking your ear, the doctor may use a small tool to remove the accumulation of dead skin cells using the method of Manual Extraction. If you feel your hearing ability is affected or have pain in the ear, you may want to consult an ENT specialist.Management and Treatment
How do I get rid of psoriasis in my ears?
- Xemsis: Formulated with the purest natural ingredients, this ointment can be effective for all types of skin conditions and has no side effects.
- Ear Drops: If your canal has an excess accumulation of dead skin cells and causes pain, your doctor may recommend ear drops with salicylic acid to remove the scales and reduce inflammation.
- Emollients: Doctors may provide moisturizers, creams, soaps, or lotions that have vitamin D and anti-inflammatory properties. Make sure that these topical treatments can be applied inside your ear canal.
- Medications: Doctors may prescribe oral drugs or biological medications if you experience severe pain and bleeding.
- Phototherapy: If psoriasis is very severe with excess inflammation and is turning into chronic psoriasis, doctors may provide ultraviolet laser therapy. The therapy is effective but has some side effects. Doctors prescribe it only for severe cases of psoriasis. Make sure of safety measures, as the skin in the ears is very sensitive.
Are there side effects of the treatment?
There will be no side effects from the treatments. But it’s important to avoid sticking any material, including cotton, fingers, or earbuds, into your ears, as the plaques may flake off and fall deep into your ear, causing hearing problems. Follow the guidelines of your doctor regularly.How soon after treatment will I feel better?
You will feel some relief from itching and discomfort right after the treatment. But it may take several weeks, or even more, to get complete relief from the symptoms. Monitor your symptoms regularly to avoid any consequences.Prevention
How can I prevent psoriasis in the ears?
There are no proven methods to prevent psoriasis in the ears. However, you can prevent the emergence of new flare-ups with some measures.- Avoid sticking fingers or earbuds to the ears
- Avoid consuming excess alcohol and tobacco products
- Identify the triggers, like sunburn and stress, and manage them effectively
- Maintain good hygiene and keep your surroundings clean
- Eat a healthy diet with more vegetables, fruits, grains, and proteins that support your immune system.
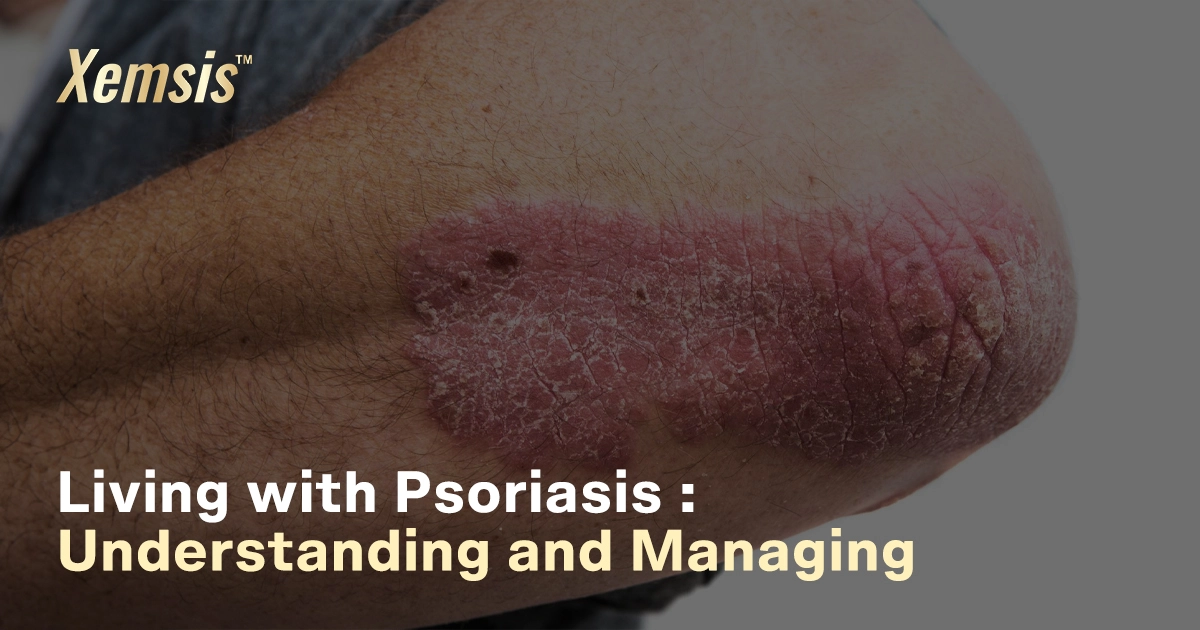
Living With psoriasis in the ears
When should I see my doctor?
Consult with your doctor without fail if:- You are experiencing hearing loss or find it difficult to hear
- There is heavy swelling, oozing of fluids, or bleeding inside the ear
- You are experiencing excess pain and itching in the affected areas
- Your symptoms are spreading to the face.
What questions should I ask my doctor?
- Ask how to follow your medications
- Ask if there is any possibility of side effects associated with the treatment
- Inquire about how to prevent plaques from entering deep into the ears
- Ask how long it would take to cure the condition completely
- Inquire about any lifestyle changes or any measures to be followed
- Inquire if there would be any need to visit an ENT specialist
Conclusion
Psoriasis in the ears is a long-lasting condition that affects the outer and inner parts of the ears. Treatments and medications work in stages to relieve you of the condition. You may feel excess pain or even have temporary hearing loss. However, consistency in following the doctor’s guidelines, following the preventive measures regularly, and keeping hope is the best option to overcome this psoriasis.Reference
- Medical News Today: https://www.medicalnewstoday.com/articles/314768#treatment
- Healthline: https://www.healthline.com/health/psoriasis/psoriasis-in-the-ears#children-and-infants
- WebMD: https://www.webmd.com/skin-problems-and-treatments/psoriasis/psoriasis-in-ears
- 4. Cleveland Clinic: https://my.clevelandclinic.org/health/diseases/24942-psoriasis-in-ears

Rakhul Mathivanan
Rakhul Mathivanan, a writer and filmmaker, focuses on creating innovative and unique content through directing short films, writing scripts, blogs, articles, case studies, and website content. He loves to watch movies, read books, listen to music, and travel. He has also had expertise in the field of writing and filmmaking for over a year and works closely with Xemsis by providing them with well-researched blogs about psoriasis.