 Categoriespsoriasis type
Categoriespsoriasis typeErythrodermic Psoriasis
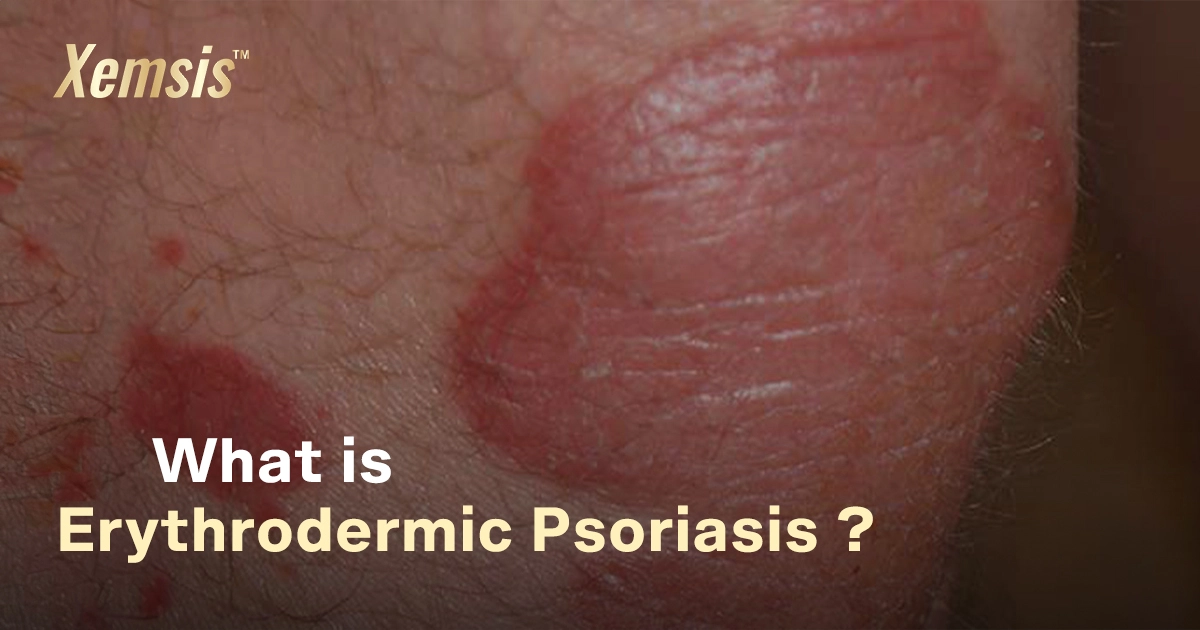
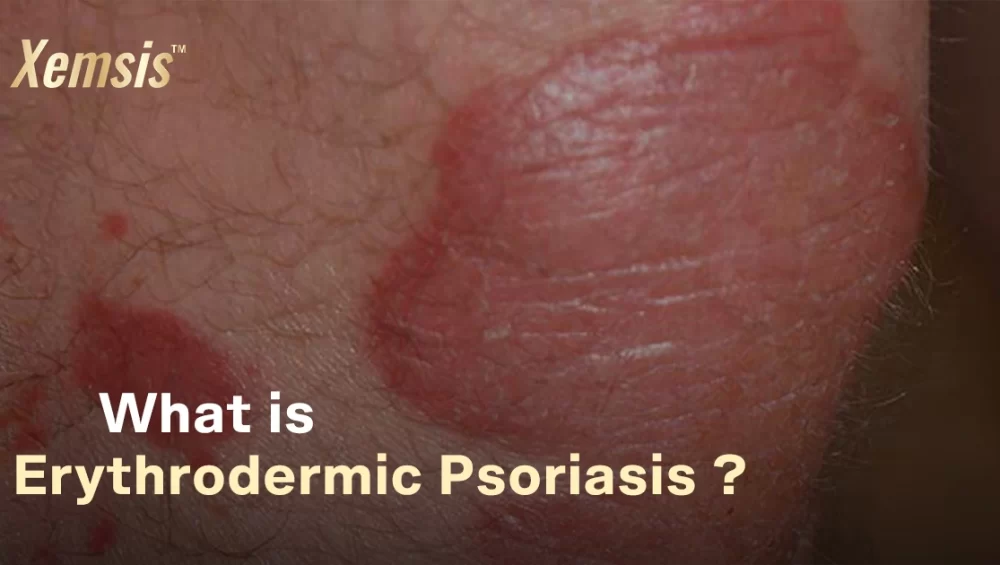
Erythrodermic psoriasis is a rare but dangerous variant of psoriasis vulgaris that causes painful and itchy red, scaly patches to spread to larger areas of skin. The condition is chronic and inflammatory, which affects the body’s ability to control the temperature. If not treated properly, this condition can be life-threatening.
Overview
What is erythrodermic psoriasis?
Erythrodermic psoriasis is a harmful type of psoriasis that causes bright and burning plaques in various regions of the body. This condition also affects the immune system, which has a higher risk of developing other complications and risk factors like heart problems and pneumonia.
The affected immune system alters the chemistry of the body and loses much-needed proteins and fluids from the body, which reduces the blood flow to the heart. If the heart doesn’t have enough blood to pump, it may fail the heart and kidney. It’s crucial to consult with doctors if you experience this condition.
How common is erythrodermic psoriasis?
Erythrodermic psoriasis is a rare type, affecting 2–3% of people with psoriasis. Also, 1 in 3 people with plaque psoriasis develop erythrodermic psoriasis. Most other forms of psoriasis are severe but not usually fatal. However, this erythrodermic psoriasis can get worse and be life-threatening if not treated properly.
Symptoms and Causes
What are the causes of erythrodermic psoriasis?
The exact cause of erythrodermic psoriasis is not proven yet. Research is going on to find the exact cause of this condition. However, the chemical process behind the condition is that it causes the immune system to overreact, which leads to the rapid production of new skin cells. For a healthy person, the skin cells usually shed and grow every 30 days. But for people with erythrodermic psoriasis, these new skin cells grow rapidly in 3 to 4 days.
The T-cells, which are responsible for attacking foreign particles in the body, malfunction and attack the healthy skin cells. As the process is very quick, the dead skin cells accumulate on the surface of the skin instead of shedding. These accumulations affect the skin, causing inflamed patches on the skin. This erythrodermic psoriasis can also easily develop from plaque psoriasis if that is not treated properly.
Other conditions that trigger erythrodermic psoriasis include:
- History of family genetics with psoriasis
- Overdosage of certain medications
- Any severe infections from microbes
- Excess stress
- Severe sunburn
- HIV
- Substance abuse.
Symptoms of erythrodermic psoriasis
- Itchy and scaly red patches spread to various areas of the body
- Extreme dehydration and fatigue
- Chills and fever
- Excess pain and burnt-looking skin
- Affected areas peel off the skin in large pieces
- Joint pain
- Rapid heartbeat
- Swelling in the lower legs and feet.
These symptoms may develop slowly or occur suddenly. Visit your doctor as soon as possible if you experience these kinds of symptoms during psoriasis.
Diagnosis and Tests
How is erythrodermic psoriasis diagnosed?
Initially, the doctor will examine your records, such as your family history, recent medications, the condition of your symptoms, your previous history of psoriasis, and infections. Then they may take a blood test to learn about your blood cells and electrolyte levels. Also, they do skin biopsy tests to confirm your condition and its severity. If erythrodermic psoriasis is confirmed, you may need to be admitted to the hospital for further treatment, as the condition is dangerous.
Management and Treatment
Erythrodermic psoriasis treatment
-
- Topical Medicines: Doctors provide effective ointments like xemsis, lotions, or corticosteroid creams that soften your plaques and reduce inflammation.
- Oral Drugs: If you have other complications with erythrodermic psoriasis, doctors may provide medications like NSAIDs, DMARDs, cyclosporine, acitretin, and etanercept that stop the immune system from attacking healthy cells and control new cell growth. These medications may have complex dosages and side effects. So doctors may recommend avoiding some food types. It’s crucial to follow their guidelines.
- Injections: To relieve you from excess pain and itching, doctors may recommend biological treatments or injections with antibiotics and pain medications.
- Stabilizing Treatments: If your physical condition is very ill with a huge loss of fluids and proteins, doctors may admit you to bed and inject IV fluids or electrolytes in your veins to make you stable.
- People with HIV: Treating erythrodermic psoriasis in people with HIV is more complicated, as usual treatments will not be effective. So first, treatments like antiretroviral therapy may be given to people with HIV.
- Phototherapy: If your erythrodermic psoriasis symptoms are fatal, doctors may recommend this phototherapy treatment. This treatment involves the process of passing ultraviolet lasers to your affected areas. The process is complex and may have some side effects.
Prevention
Can you prevent erythrodermic psoriasis?
There are no proven measures to prevent erythrodermic psoriasis. However, there are some ways to prevent new flare-ups.
- Apply Xemsis regularly, as prescribed
- Avoid consuming alcohol and tobacco products
- Manage stress with meditation and yoga
- Protect your skin from external injuries like cuts, burns, infections, or wounds
- Keep in touch with your healthcare provider
- Don’t abruptly stop previous medications or try new medications.
- Eat a healthy diet and stay hydrated
- Protect yourself from harsh weather, be it summer or winter.
Conclusion
Erythrodermic psoriasis can be very challenging, affecting your physical strength and appearance. Treating this type of psoriasis involves many trials and errors. You will need to change your lifestyle and take medications for long periods of time, as they work in stages to relieve you of the condition. This condition can be life-threatening if it is not treated properly. So it’s crucial to follow your doctor’s guidelines and stay positive.
Reference
- WebMD: https://www.webmd.com/skin-problems-and-treatments/psoriasis/erythrodermic-psoriasis
- National Library of Medicine: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5572467/
- Healthline: https://www.healthline.com/health/erythrodermic-psoriasis#outlook
- Medical News Today: https://www.medicalnewstoday.com/articles/314514#takeaway
- National Psoriasis Foundation: https://www.psoriasis.org/erythrodermic-psoriasis/
- HIVinfo: https://hivinfo.nih.gov/understanding-hiv/fact-sheets/hiv-treatment-basics
- Cleveland Clinic: https://my.clevelandclinic.org/health/diseases/22998-erythrodermic-psoriasis

Rakhul Mathivanan, a writer and filmmaker, focuses on creating innovative and unique content through directing short films, writing scripts, blogs, articles, case studies, and website content. He loves to watch movies, read books, listen to music, and travel. He has also had expertise in the field of writing and filmmaking for over a year and works closely with Xemsis by providing them with well-researched blogs about psoriasis.